The literature review on Cataract management in children
Congenital and childhood cataracts are uncommon; however, most paediatric ophthalmology units in the UK see them regularly. They’re frequently linked to severe vision loss, and a vast percentage have a genetic cause, with some having extra-ocular severe comorbidities. In most cases, optimal diagnosis and treatment necessitate close coordination across multidisciplinary teams. Surgery is still the most communal form of therapy. Many surgical procedures, intervention dates, and optical correction choices have been promoted, making care seem complicated to those who regularly encounter affected children. This report summarises the outcomes of two recent RCOphth child cataract study days, Offers a Literature Review, and discusses the current state of play’ in paediatric cataract therapy in the United Kingdom.
Introduction
Congenital cataract (CC) affects between 2.2 and 13.6 people worldwide. The difference in frequency amongst populations is likely owing to higher detection rates in countries with screening programmes (for both cataracts and problems related to cataracts), lower rubella vaccination rates, and population genetic differences. Treatment is also different depending on whether you have thick cataracts at birth, partial cataracts at birth, or developmental cataracts that develop during childhood. Early recognition, diagnosis, and proper treatment are critical for attaining the best possible results. A team of healthcare earners is often involved in the best management of children with cataracts, and clinical networks and well-established referral pipelines are crucial for achieving the best results. Management has improved rapidly in recent decades, from diagnosis to surgical procedures; however, there is still heterogeneity in treatment in the United Kingdom. We examine the literature and give consensus from five big specialised centres in the UK in this study to assist clinicians in managing children with this rare but critical disorder[1].
PhD Assistance develops Medical coding systems using ICD-10-CM, CPT® framework and many more to booth secure access control in Networking platforms. Hiring our experts, you are assured of quality and on-time delivery.
CLINICAL TIP: The optimal time to operate on a newborn with a visually significant cataract is within the first few weeks of life. As a result, babies detected with potential CC by non-specialist screening measures should be sent to specialists as soon as feasible to confirm the diagnosis. Referral to a specialised paediatric cataract service should be treated with the same urgency.
Hire PhD Assistance experts to develop your algorithm and coding implementation for your medical research dissertation Services.
Diagnostic workflow for children with CC
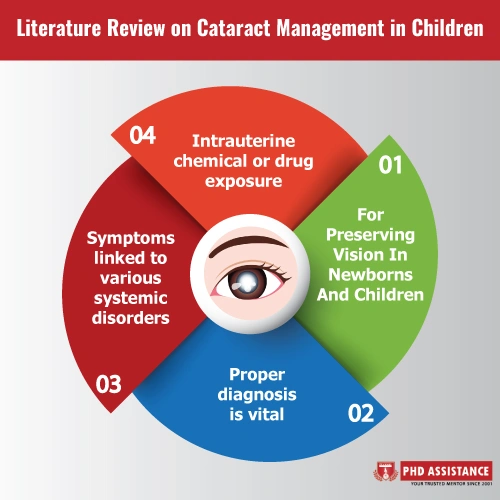
While early detection and surgical intervention are critical for preserving vision in newborns and children, proper diagnosis is vital. CC is a condition with a wide range of symptoms linked to various systemic disorders. Trauma, maternal TORCHS infection (toxoplasmosis, rubella, CMV, herpes simplex, and syphilis), intrauterine chemical or drug exposure, metabolic imbalance, and genetic variation are possible causes (chromosomal abnormalities or single gene mutation associated disorders). Even with clinical algorithms, determining a diagnosis is difficult and time-consuming. Traditionally, doctors have pursued biochemical, genetic, clinical, and imaging studies sequentially or iteratively. This method relies on accurate clinical phenotyping, entails many clinical professionals and appointments, and comes at a high expense to patients and healthcare providers, all while yielding a low diagnosis rate.
During surgery
Basic surgical techniques
A general anaesthetic is required for cataract surgery in children, and it should be preceded by a similar anaesthetic examination of both eyes (EUA). Biometry (contact and keratometry or immersion A-scan ultrasonography) is used intra-operatively in younger children and pre-operatively in older children to assess IOL or CL power utilising non-contact biometry (e.g. IOL Master). The child’s age determines the surgical procedure and whether an IOL is implanted. A vitrectomy cutter can nearly always aspirate or remove the lens, and this is followed by a cefuroxime intracameral injection and a subconjunctival or intracameral steroid injection. Some surgeons leave a CL in place after surgery to rectify the aphakic refractive defect. CLs in the best shape 1–2 weeks after surgery [2].
PhD Assistance experts have experience handling dissertation and medical research assignments with assured 2:1 distinction. Talk to Experts Now
After surgery
Post-operative eyedrop regimes in paediatric cataract surgery
Young children’s post-operative inflammatory reactions are more intense than those of older children and adults, and they are influential in newborns and those with uveitic cataracts. This can result in discomfort, creating the pupillary membrane and posterior synechiae, pupil-block glaucoma, and IOL deposits and decentration. In youngsters, post-operative endophthalmitis has a bad prognosis. Using post-operative drops after cataract surgery in children aims to minimise inflammation and infection risk in combination with intraoperative antibiotics.
Risk factors
Clinical studies have revealed that surgery at a younger age increases the risk of glaucoma. According to some studies, glaucoma is four times more likely if surgery is performed before the period of four weeks, with glaucoma occurring only if surgery is performed between the ages of six and nine months, with a 2% reduction in risk for each additional week of age at surgery.
Management
Medical therapy can keep GFCS under control for years, and it’s more likely to keep surgery off the table in later-onset instances. A safe, non-overburdening, and cost-effective treatment regimen should be adopted. Except for Latanoprost, most glaucoma drugs are not approved for use in children, and this should be discussed with parents before prescription and the rationale for the pharmaceutical decision.
There are many sensible topical treatment combinations. A reasonable topical treatment escalation, with progression to the next step in the context of inadequate pressures, is given here:
- (i) Latanoprost or timolol 0.25% monotherapy.
- (ii) Combination dorzolamide/timolol preparation.
- (iii) Dorzolamide/timolol combination plus latanoprost.
CLINICAL TIP: Although technically challenging, there is now a range of surgical options available for secondary IOL implantation in children enabling successful long-term optical and visual rehabilitation. Considering IOL implantation in aphakic children, mainly those intolerant of CL wear or glasses, is an option at any age after early infancy[3].
Summary
Paediatric cataracts (CC) are a prevalent and severe cause of lifetime vision loss in children. Affected newborns should be handled by specialised services with the necessary competence and infrastructure. The way children with CC are evaluated and treated has altered thanks to advances in genetics substantially, and early intervention is typically the key to achieving the best possible results for these children.
PhD Assistance has vast experience in developing dissertation research topics for students pursuing the UK dissertation in Medical research. Order Now
References
- Wu X, Long E, Lin H, Liu Y. Prevalence and epidemiological characteristics of congenital cataract: a systematic review and meta-analysis. Sci Rep. 2016;6:28564.
- Trivedi RH, Wilson ME. Selection of an initial contact lens power for infantile cataract surgery without primary intraocular lens implantation. Ophthalmology. 2013;120:1973–6.
- Self, J. E., et al. “Cataract management in children: a review of the literature and current practice across five large UK centres.” Eye 34.12 (2020): 2197-2218.



